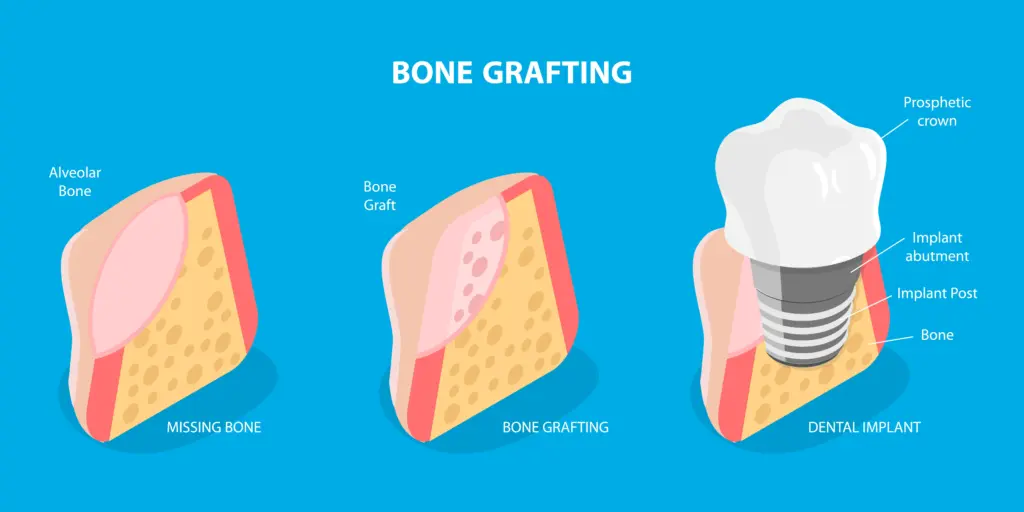
Replacing a missing tooth is about more than a visible gap. Teeth rely on a healthy jawbone for support. When bone becomes thin or hollow, treatments such as dental implants may not be possible immediately. A dental bone graft rebuilds or strengthens the jaw so it can support a replacement tooth securely.
This guide explains what a graft involves, when it is advised, what to expect during treatment, and how to look after yourself while you heal.
Why might you need a bone graft?
Bone is a living tissue that adapts to use. After a tooth is lost, the jaw in that area no longer receives routine chewing forces. Without this stimulus, the ridge can lose width and height. A graft may be recommended to:
- Prepare for an implant when scans show the jaw is too thin or soft for secure placement. If you are considering this route, you can explore options on our dental Implants page.
- Address long-standing tooth loss where the ridge has reduced.
- Repair areas affected by gum disease or past infection.
- Restore defects after an injury.
- Improve the fit of a denture by reinforcing the ridge.
The aim is a stable, healthy foundation so your final restoration looks natural and functions well.
What is placed during a bone graft?
A graft introduces a carefully selected material to the area where bone is needed. The material acts as a scaffold. Your own bone cells grow across it and gradually replace it with living bone. For a clear overview of how grafting fits into implant care, see the Guy’s and St Thomas’ dental implants patient information.
Types of graft material
Your dentist will suggest the most suitable option based on your scan, medical history and treatment goals.
- Autograft
Bone from your own jaw. It contains living cells and natural growth factors. - Allograft
Donor human bone that is processed and sterilised to high medical standards. It avoids a second surgical site. - Xenograft
Bone from another species, commonly bovine. Processing leaves a mineral framework that supports your bone to grow. - Alloplast
A synthetic, biocompatible option designed to integrate with your bone.
At a glance: graft choices
| Graft type | Source | Advantages | Considerations | Typical uses |
| Autograft | Your jaw | Excellent compatibility and healing potential | Second surgical site and limited supply | Localised defects and younger patients |
| Allograft | Donor human bone | No second site and good availability | Very rare immune response | Ridge preservation and general augmentation |
| Xenograft | Bovine origin | Holds shape and resorbs slowly | May remain longer as a scaffold | Sinus lifts and larger defects |
| Alloplast | Synthetic | Consistent quality and no donor needed | May integrate more slowly in some cases | Socket preservation and small to medium defects |
When is a graft performed?
Timing depends on your needs and the planned restoration.
- Socket preservation at extraction helps protect the ridge shape for future planning.
- Delayed grafting, some months after extraction, is used when the ridge has already thinned.
- Sinus lift in the upper back jaw raises the sinus floor to create height for an implant. The approach is outlined in the Cambridge University Hospitals sinus lift guide.
- Ridge augmentation widens or increases the height where bone has reduced over time.
If you want to see how a graft sits within the wider journey, our step-by-step overview is here: what to expect during the dental implant process.
What happens during the procedure?

Most grafts are carried out under local anaesthesia in a dental surgery. Many people describe pressure rather than pain. Sedation can be arranged if you feel anxious.
- Assessment and planning
A full examination and a 3D scan measure bone, map nearby structures and guide precise placement. - Anaesthetic and site preparation
The area is numbed and gently prepared. If a tooth needs removal, this is performed first using techniques that conserve bone. - Placing the graft
The chosen material is placed into the prepared site. A fine membrane may be added to protect the graft and guide healing. - Suturing
The gum is closed with small stitches. These may dissolve or be removed at review. - Aftercare and review
You receive tailored instructions and a follow-up to check healing.
Procedure time varies with complexity. Many straightforward cases take between 45 and 90 minutes.
Good to know: If there is strong initial stability, an implant can sometimes be placed at the same appointment as a minor graft. In other cases, the graft is allowed to mature first because this offers a more predictable outcome.
Is a bone graft painful?
You should be comfortable during treatment due to the local anaesthetic. Mild tenderness, swelling and minor bruising for a few days are common. Most patients manage with over-the-counter pain relief. A wrapped cold pack in short intervals during the first day helps with swelling. Sleeping with your head slightly raised for a night or two can be useful.
How long does healing take?
Healing has two phases.
- Early healing covers the first one to two weeks as the gum seals and stitches dissolve or are removed.
- Bone remodelling continues for several months as your bone cells replace the graft and strengthen the site.
For implants, many cases wait three to six months before placement. Larger reconstructions may need longer. A follow-up scan confirms when the site is ready.
Benefits and possible risks
Benefits
- Restores volume so an implant or denture has reliable support.
- Helps shape a natural gum contour around future teeth.
- Can reduce the chance of further bone loss in the grafted area.
Possible risks
All surgery carries some risk, though problems are uncommon with careful planning and good home care. The hospital leaflet from Guy’s and St Thomas’ summarises common effects and rare complications.
- Infection or delayed healing
- Minor bleeding or bruising
- Exposure of the graft or membrane that needs attention
- Graft not integrating as expected
- Temporary sinus-related symptoms after a sinus lift
Your dentist will explain how your personal risk is minimised and the signs to report during recovery.
Looking after yourself after a bone graft
Good aftercare supports success. Follow the instructions from your dental team and keep the area undisturbed while it settles.
The first 24 to 72 hours
- Protect the site
Do not touch the graft with your fingers or tongue, and avoid pulling your lip to check stitches. - Manage bleeding
A small amount of oozing is normal. Use the provided gauze if needed and rest with your head slightly elevated. - Choose soft, cool foods
Yoghurt, smoothies, scrambled eggs, mashed potatoes and soups that are not hot work well. - Avoid hot drinks and alcohol
Heat can encourage bleeding, and alcohol may slow healing. - No smoking or vaping
Nicotine reduces blood flow and increases the risk of graft failure. The NHS Better Health quit smoking hub offers proven methods and local support. - Pain relief as directed
Take medication as advised and do not exceed the stated dose.
From day three onwards
- Gentle brushing with a soft toothbrush, keeping clear of stitches.
- Antibacterial mouth rinse, if prescribed, usually starts after 24 hours.
- Normal activities as you feel able, while avoiding heavy exercise for a few days.
- Food choices that avoid crunchy textures, seeds and nuts, which might disturb the area.
Can an implant be placed at the same time?
Sometimes. If the initial hold is strong, an implant may be placed at the same appointment as a small graft. More often, the graft is allowed to mature first, and an implant is placed later into the strengthened site. Your scan and clinical findings guide the decision. For timings and suitability tailored to you, contact us.
Frequently asked questions
Will other people notice I have had a bone graft?
Unlikely. Any swelling is usually mild and short-lived. Stitches are hidden inside the mouth. Many people return to work the next day, depending on their role.
What if I am nervous about treatment?
Tell your dentist. Calm appointments, clear explanations and sedation where appropriate can make the experience much easier. Bringing a supportive friend or family member can help.
Is a bone graft safe?
Yes. It is established in UK practice and carried out in line with professional and hospital guidance. The Cambridge University Hospitals sinus lift guide explains one of the most common techniques in plain language.
How do I know if I am suitable?
A consultation and 3D scan confirm suitability. Even with significant bone loss, there are reliable ways to rebuild volume for a long-lasting result. If you want to see how grafting fits into the journey, review what to expect during the dental implant process and discuss options with the team.
Quick guide: choices and healing
- Socket preservation
Usually completed at extraction. Typical wait before implant placement is three to four months. - Ridge augmentation
Used where the ridge has thinned. Healing before implant placement is often four to six months or more. - Sinus lift
Raises the sinus floor in the upper back jaw. Healing before implant placement is usually six to nine months, depending on the amount of lift.
Final thoughts
A dental bone graft is a steady and well-tested way to rebuild the foundation for a secure replacement tooth. With careful planning, skilled hands and sensible aftercare, most patients heal smoothly and regain confident chewing and a natural-looking smile. If your scan shows thinning bone, there are dependable techniques to restore volume and set you up for long-term success with your chosen treatment.




